Approximately 40% of the worldwide population suffer from unexplained gut problems [1], which contribute to a poor quality of life. Despite such a large proportion of society suffering from their gut health, as well as the economic strain on society from this condition, diagnostic and treatment pathways are limited.
The time from first seeing a doctor for digestive health complaints to successfully being diagnosed with a digestive condition can be very long. Many people suffer for extended periods of time while they search for answers, and the light at the end of the tunnel can seem out of reach.”
There are currently a wide range of diagnostic tests used by gastrointestinal consultants, ranging from blood and stool tests, to endoscopic procedures but these tests are often uncomfortable and painful for the patient. A simple breath test for gut problems is one of the diagnostic tools available and is a non-invasive alternative, meaning the patient can be at ease and comfortable during the process.
In our previous blogs, we have discussed how a Hydrogen Methane Breath Test (HMBT) works. A short summary is: bacteria in the colon normally produce hydrogen and methane when digesting sugars. These gases are then transferred into the bloodstream and transported into the lungs, before being exhaled on breath. If there are higher levels of hydrogen and methane, it could be inferred that colonic bacteria have colonized the small intestine, and are digesting sugars far earlier in the intestinal tract than is normal.
This is known as small intestinal bacterial overgrowth (SIBO), and is associated with uncomfortable symptoms such as bloating. However, this poses the question, how do you know how much hydrogen or methane is too much?
What is the North American Consensus (NAC) and how will it help in testing my gut problems?
With the popularity of breath tests for digestive diseases and other gut problems growing, yet the concerns and criticisms of this method remaining, the NAC was developed. Informed by experimental work and expert opinion, a consortium of specialists published the NAC consisting of 26 guidelines, with the aim to provide a standardized process for the optimal interpretation of HMBTs [2].
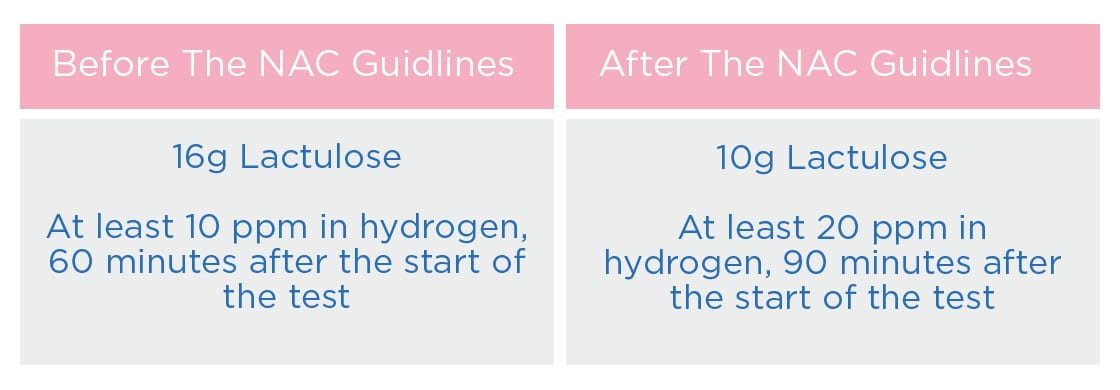
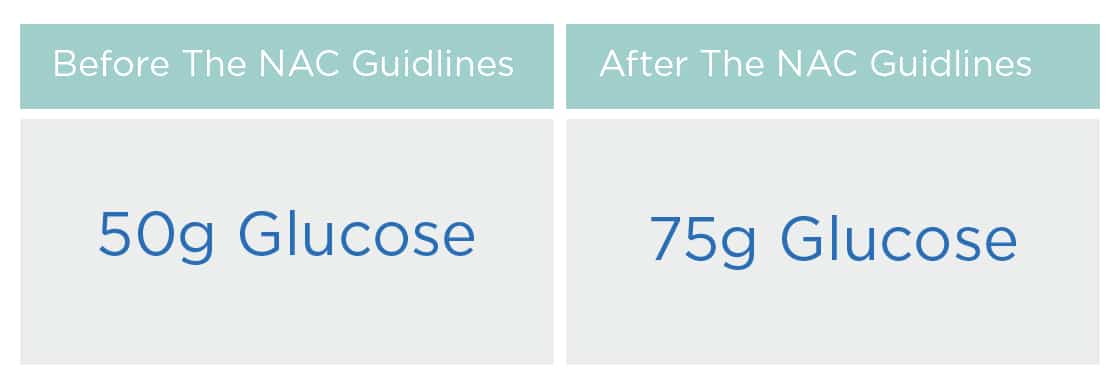
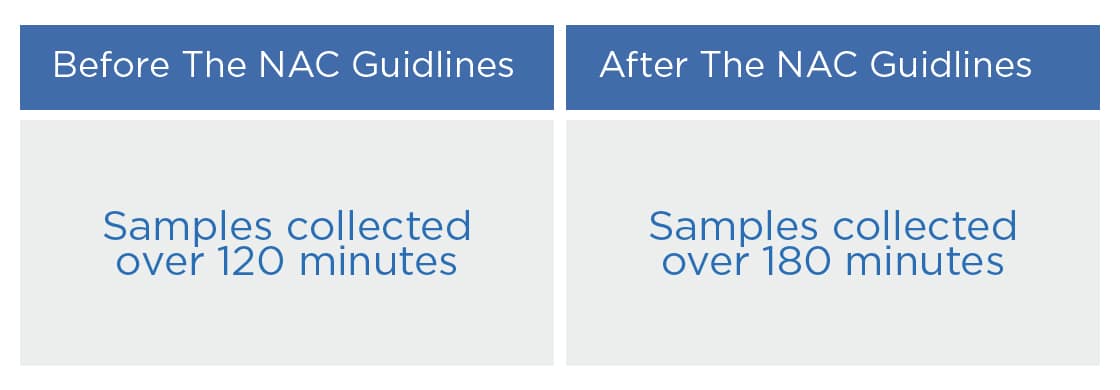
The NAC in turn proposed several changes to the tests, with the goal of improving the accuracy of results and providing greater consistency across test providers. As part of an HMBT, patients are required to drink a substrate diluted in water. The NAC changed the criteria for some of the tests, including lowering or raising the dosage of the substrate, the benchmarks for the parts per million on breath, as well as the duration of sampling.
A recent study by Pitcher et al., compared HMBT results based on the NAC to previous methods prior to the guidelines [3].
Did the changes work?
The most common test uses the indigestible sugar, lactulose, to detect SIBO. Lactulose is often used as a laxative, which can decrease transit time in the small bowel [4]. This means that the substrate may get into the colon faster and produce a colonic peak in hydrogen and methane, which could be mistaken for a small bowel peak. Not only could this leave the patient in some discomfort, but it could end with a false positive result.
To reduce these risks the NAC for SIBO reduced the dose of lactulose, and increased parts per million of hydrogen that had to be detected for a positive result, as well as extended the sampling time. Pitcher et al. found that the lower dose of lactulose was favored, with patients less likely to suffer from symptoms and/or receive a false positive result.
If the lactulose substrate is not suitable for a patient, SIBO can also be detected using glucose as a substrate. Unlike lactulose, glucose is rapidly absorbed in the upper intestine meaning it has the potential for false negatives. The changes to the NAC for SIBO increased the glucose dose to 75g, aligned with the dose typically used for diabetes testing. The higher dose of glucose resulted in more positive results (22.2% vs 35.8%). The higher glucose dose came with a side effect of some gut problems including increased nausea experienced by patients; yet, this was only observed in those who ended up receiving a positive test result for SIBO.
This means that the increased nausea appeared to be a consequence of SIBO-related pathology. Despite nausea being an unpleasant symptom, the increased diagnostic accuracy gained from using 75g of glucose seems to outweigh the higher risk of a false negative associated with using a lower dose of glucose.
In some cases, a specialist may also suggest you take a lactose or fructose test, used to test for carbohydrate malabsorption. To increase standardization and improved diagnostic performance, the NAC suggested collecting breath samples over a longer period, increasing the overall sampling time by 60 minutes.
How do we align with the NAC Guidelines
The research from Pitcher et al., states that by relying on comparison of the occurrence and severity of symptoms, these results broadly support the widespread use of the NAC guidance for the clinical application of HMBTs for SIBO and carbohydrate malabsorption.
Additionally, it proposes the use of multiple criteria for determining positive results in lactulose breath tests, indicating that this can help to identify borderline cases and inform more robust decision making in relation to patient care [3]. It is crucial that the tests and analysis that we provide are aligned with the recommendations given by the NAC to help patients find the answers that they are looking for or rule out SIBO or carbohydrate malabsorption. The main treatment for SIBO is a course of antibiotics, yet with the global problem of bacterial resistance to antibiotics, it is crucial that a correct diagnosis is given for the most appropriate treatment pathway.
If you would like to find out more about hydrogen methane breath tests for your gut problems or keep up to date with our latest news, take a look at our Insights Hub.
Or, if you are ready to get started and try an HMBT for yourself, complete the form on our website.
References:
-
Sperber et al. (2020) Worldwide Prevalence and Burden of Functional Gastrointestinal Disorders, Results of Rome Foundation Global Study Gastroenterology 160:99–114. DOI: 10.1053/j.gastro.2020.04.014
-
Ghoshal UC, Ratnakar Shukla, Ghoshal U. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome: A Bridge between Functional Organic Dichotomy. Gut Liver. 2017. 11(2): 196-208. DOI: 10.5009/gnl16126
-
Pitcher CK, Farmer AD, Haworth JJ, Treadway S, Hobson AR. Performance and Interpretation of Hydrogen and Methane Breath Testing Impact of North American Consensus Guidelines. Digestive Diseases and Sciences. 2022. DOI: 10.1007/s10620-022-07487-8
-
Yu D, Cheeseman F, Vanner S. Combined oro-caecal scintigraphy and lactulose hydrogen breath testing demonstrate that breath testing detects oro-caecal transit, not small intestinal bacterial overgrowth in patients with IBS. Gut. 2011 Mar;60(3):334-40. doi: 10.1136/gut.2009.205476