What is IBS and how many people does it affect
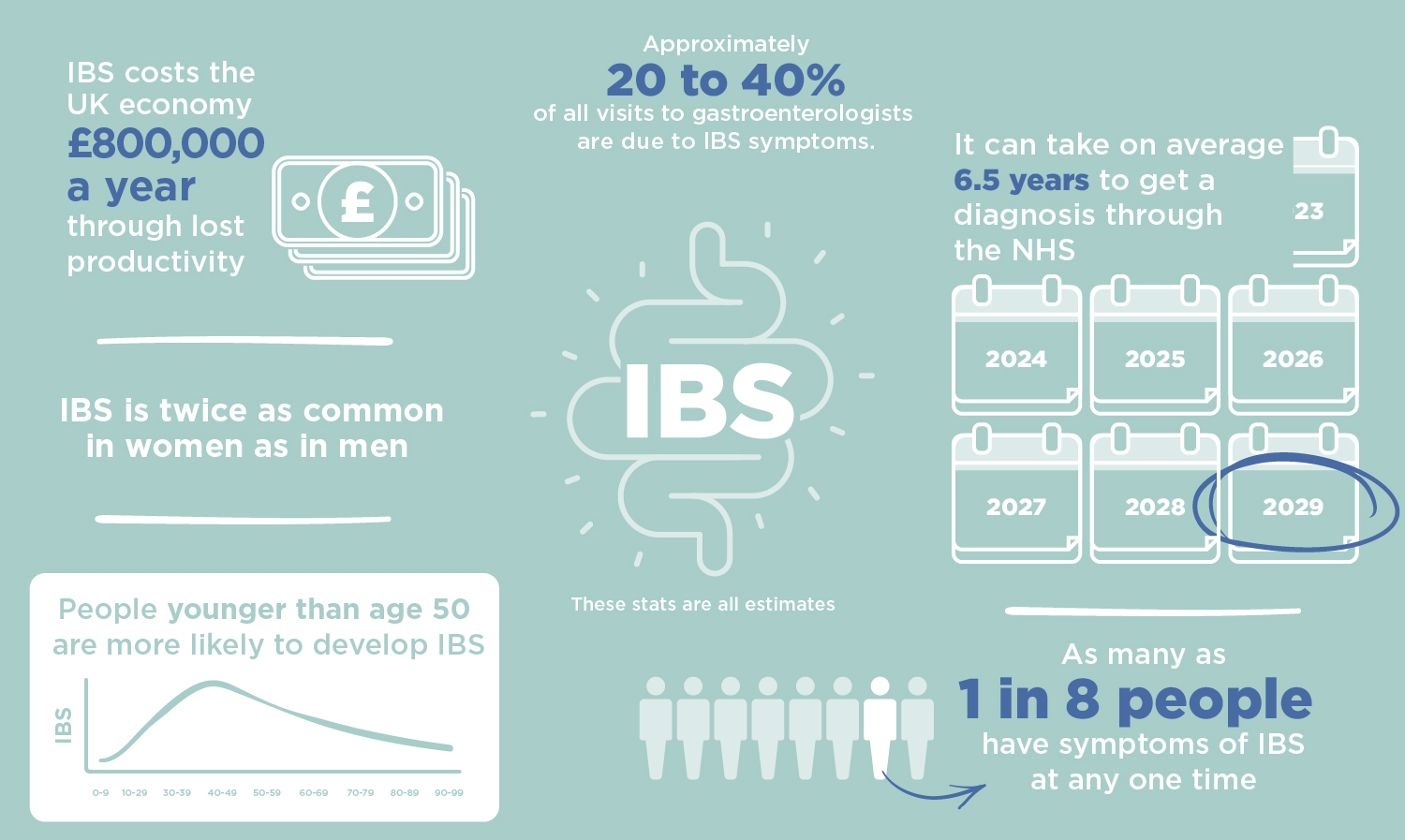
Irritable Bowel Syndrome (IBS) is one of the most common gastrointestinal conditions – thought to affect up to one in five of us during our lifetimes, and it is one of the most frequent reasons for someone to receive a referral to a gastroenterology clinic (1). IBS is an umbrella term that describes a broad range of digestive symptoms, such as pain, cramping, and irregular bowel movements that can significantly reduce quality of life. Despite how common it is, IBS is still a misunderstood condition, with patients commonly reporting feeling unsupported.
Based on the specific symptoms experienced, there are four subtypes of IBS. These four types are IBS-D (mostly diarrhea), IBS-C (mostly constipation), alternating diarrhea and constipation (IBS-mixed), and IBS-U, where symptoms are highly variable. Despite its prevalence and life-limiting symptoms, there are no specific tests or physical changes that can be used for a concrete diagnosis of IBS. Instead, a diagnosis of IBS is usually made after a series of clinical tests rule out other conditions, such as inflammatory bowel disease (IBD), coeliac disease, or cancer. As mentioned in some of our other blog posts, digestive symptoms heavily overlap between different gut disorders, therefore ruling out more serious conditions is a very important process.
After an often seemingly endless sequence of doctor visits and tests, if a diagnosis of IBS has been given, patients can feel like they have been left to deal with the frustrating and life-limiting symptoms alone, as there is little clear treatment or guidance available. This context makes it no surprise that many turn to fad cures and may progressively restrict their diet over time out of desperation to lessen some of the symptoms. However, endlessly restricting the diet in a desperate attempt to reduce some of the digestive discomfort without the guidance of clinicians and a systematic plan is not advisable, and is often not productive in finding solutions. In extreme scenarios, this can put IBS sufferers at risk of developing an eating disorder known as avoidant/restrictive food intake disorder (ARFID). This disorder is characterized by a loss of enjoyment of food, seeing it merely as a means to get sustenance, and sufferers can even become underweight and nutrient-deficient (2,3). Crucially, IBS patients are twice as likely to have ARFID as those without IBS, and there is a clear link between diet restriction and progressively avoidant behavior towards food (4,5). You must always speak to your doctor before making large changes in the diet, and often dietary changes such as the FODMAP diet are recommended as temporary measures to better understand your individual triggers.
What causes IBS
So, what causes IBS in the first place? One of the major reasons that IBS is difficult to diagnose and treat is that it has a complex and not completely understood mechanism, with many potential contributing factors that can underpin the symptoms. Some of these factors include the gut microbiome, infection, changes to the muscle contractions of the intestines, hormonal changes, stress, mood disorders like depression or anxiety, and food intolerances. The symptoms of IBS are very strongly linked with psychological factors, with about 85% of IBS sufferers also reported to have conditions such as anxiety and depression (6) – so much so that it was once thought that IBS was purely a psychosomatic condition. The condition is now understood to be much more complex than this, with psychological factors relating to the root cause of the gastrointestinal symptoms through the gut-brain axis – unfortunately there is still a lack of conclusive information for this aspect of the condition, and how this could inform treatment options.
It is important to note that it has been estimated that many people who have been diagnosed with IBS, may in fact have a different underlying gut condition with very similar symptoms. These include small intestinal bacterial overgrowth (SIBO), intestinal methanogen overgrowth (IMO), or carbohydrate malabsorption (CM). There appears to be a strong link particularly between SIBO and IBS, with more IBS sufferers testing positive for SIBO than those without IBS, and there may be underlying causes to both conditions (i.e. having IBS may predispose you to SIBO, or vice versa) (7). However, unlike IBS, there are more well-established diagnostic and treatment guidelines for SIBO, and CM, as we have a deeper scientific understanding of the mechanisms that cause these conditions.
How can breath testing help
Receiving a diagnosis of IBS can be long and difficult, but ruling out more serious conditions is important. Once you have received a diagnosis of IBS, due to the complex nature of the disorder, what helps one person may not help you, but where do you start? First of all, the ideal situation to finding solutions to the difficult symptoms of IBS is having a solid patient-physician relationship (1), as a systematic approach to ruling out specific triggers and causes is crucial. When this is not possible, building a network of experts such as dietitians that can help you to understand your unique situation is best. When the gut microbiome is suspected to be involved, the levels of hydrogen and methane in your breath can provide insight alongside your symptoms to monitor the success of certain treatments. The levels of these key gases can also be used by your clinician to diagnose the presence of certain conditions like SIBO, that may be contributing to your digestive symptoms. Interestingly, IBS-C (the subtype with constipation as the dominant symptom) has been associated with excessive methane in the breath (8), so monitoring the levels of methane in your breath could be useful to track your progress with different treatments if this is the type of IBS you experience.
How to test for IBS at home?
Many people experiencing IBS-like symptoms — including bloating, abdominal pain, or irregular bowel habits, may actually have SIBO (small intestinal bacterial overgrowth) or IMO (intestinal methanogen overgrowth).
The OMED Health SIBO Test allows you to test conveniently from home. Each kit includes the OMED Health Breath Analyzer, the App, and doctor-reviewed results to provide a clear diagnosis.
For a complete approach to treatment, our Gut Reset+ Plan combines SIBO testing, antimicrobial treatment, and doctor support to help restore gut balance and improve symptoms, all in one end-to-end program.
OMED Health gives you the tools and expertise to understand your gut and take meaningful steps toward long-term digestive health.
References
- Soares RL. Irritable bowel syndrome: A clinical review. World J Gastroenterol. 2014 Sep 14;20(34):12144–60. DOI: 10.3748/wjg.v20.i34.12144
- American Psychiatric Association, American Psychiatric Association, editors. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington, D.C: American Psychiatric Association; 2013. 947 p.
- Administration SA and MHS. Table 22, DSM-IV to DSM-5 Avoidant/Restrictive Food Intake Disorder Comparison [Internet]. Substance Abuse and Mental Health Services Administration (US); 2016 [cited 2023 Aug 23]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519712/table/ch3.t18/
- Harer K, Baker J, Reister N, Collins K, Watts L, Phillips C, et al. Avoidant/Restrictive Food Intake Disorder in the Adult Gastroenterology Population: An Under-Recognized Diagnosis?: 417. Official journal of the American College of Gastroenterology | ACG. 2018 Oct;113:S247. DOI: 10.14309/00000434-201810001-00417
- Simons M, Taft T, Doerfler B, Ruddy J, Bollipo S, Nightingale S, et al. Narrative review: Risk of eating disorders and nutritional deficiencies with dietary therapies for irritable bowel syndrome. Neurogastroenterology & Motility. 2022;34(1):e14188. DOI: 10.1111/nmo.14188
- Kawoos Y, Wani ZA, Kadla SA, Shah IA, Hussain A, Dar MM, et al. Psychiatric Co-morbidity in Patients With Irritable Bowel Syndrome at a Tertiary Care Center in Northern India. J Neurogastroenterol Motil. 2017 Oct;23(4):555–60. DOI: 10.5056/jnm16166
- Ghoshal UC, Shukla R, Ghoshal U. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome: A Bridge between Functional Organic Dichotomy. Gut Liver. 2017 Mar;11(2):196–208. DOI: 10.5009/gnl16126
- Hwang L, Low K, Khoshini R, Melmed G, Sahakian A, Makhani M, et al. Evaluating breath methane as a diagnostic test for constipation-predominant IBS. Dig Dis Sci. 2010 Feb;55(2):398–403. DOI: 10.1007/s10620-009-0778-4




