The current craze around probiotics for gut health is everywhere – but do these microorganisms really make it to the right place in your gut? In this blog, we will explain what they are, what happens when we ingest them, and what are the proposed health benefits.
Probiotics and Their Benefits
There is a community of microbes that normally live in our gut, known collectively as the gut microbiome. Some of these are beneficial to us, although others can be harmful, especially if they become unbalanced (also known as dysbiosis). This fluidity in terms of ‘good’ and ‘bad’ microbes can sometimes make it difficult to diagnose an unbalanced gut, or even tell what is normal. In order to be called a probiotic, certain strains of bacteria, yeast or other microbes must have an overall positive effect on the body when ingested.
By definition, probiotics are “live microorganisms which when administered in adequate amounts confer a health benefit on the host” (1).
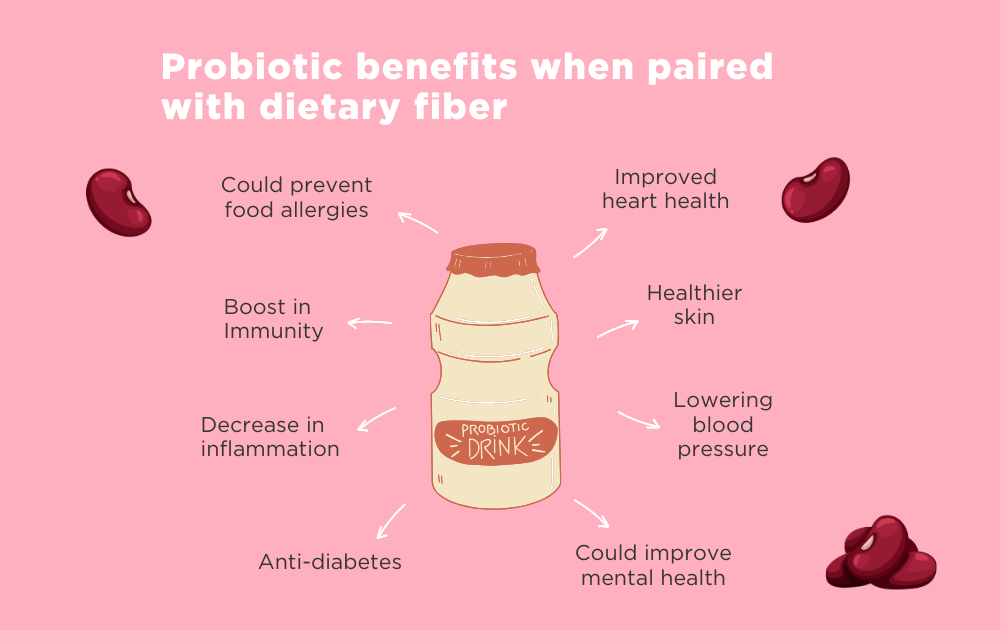
Most people already have some beneficial bacteria in their large intestines. They break down dietary fibers that we cannot digest on our own and have been linked to a variety of specific health benefits (2), these include:
- Reducing inflammation (3)
- Helping regulate the immune system (4)
- Reducing the probability of developing certain cancers (5)
- Protecting against developing diabetes (6)
- Improving heart health (7)
An important factor concerning gut microbiome health is microbial diversity. Having a higher number of different types of microbes in the gut has even been linked to improving the skin and mental health. However, some types of microbes can make us sick and they tend to feed on refined sugars and saturated fats (8). This is why eating a balanced diet of mostly whole foods is the best way to maintain a healthy gut microbiome.
Where You Can Find Probiotics
Probiotics can be found in a variety of yoghurts, fermented foods (like kefir or kimchi), or as over-the-counter pills and powders to be mixed with water. Increasing your intake of probiotics can boost numbers of beneficial microbes which leaves less space for potentially harmful ones to proliferate. Thus, probiotics can help to balance the gut, keeping the body working as it should.
Boosting the gut with probiotics is sometimes recommended by healthcare professionals. For example, taking a course of antibiotics can kill off large numbers of beneficial microbes as well as harmful ones.
Other factors that can kill probiotics:
- Exposure to heat
- Acidic conditions
- Alcohol
- Anti-microbial substances and medications
Have you heard of Saccharomyces boulardii? Small intestine bacterial overgrowth (SIBO) is caused by dysbiosis, where the gut microbiome becomes imbalanced. Interestingly, studies have shown that dysbiosis symptoms can be improved using probiotics like Saccharomyces boulardii for SIBO treatment (9) (10). It is important to remember that the individual strains of bacteria found in probiotics and their abundance is different depending on the product and should be chosen in accordance with the individual’s gut microbiome and their specific dysbiosis. For example, someone with traveler’s diarrhea would most probably need a different treatment option to someone suffering with irritable bowel syndrome (IBS). It’s best to speak to a doctor to help you choose the best option for you.
You may have also heard of another supplement called prebiotics. Find out more about prebiotics in our blog.
How Probiotics Survive Stomach Acid
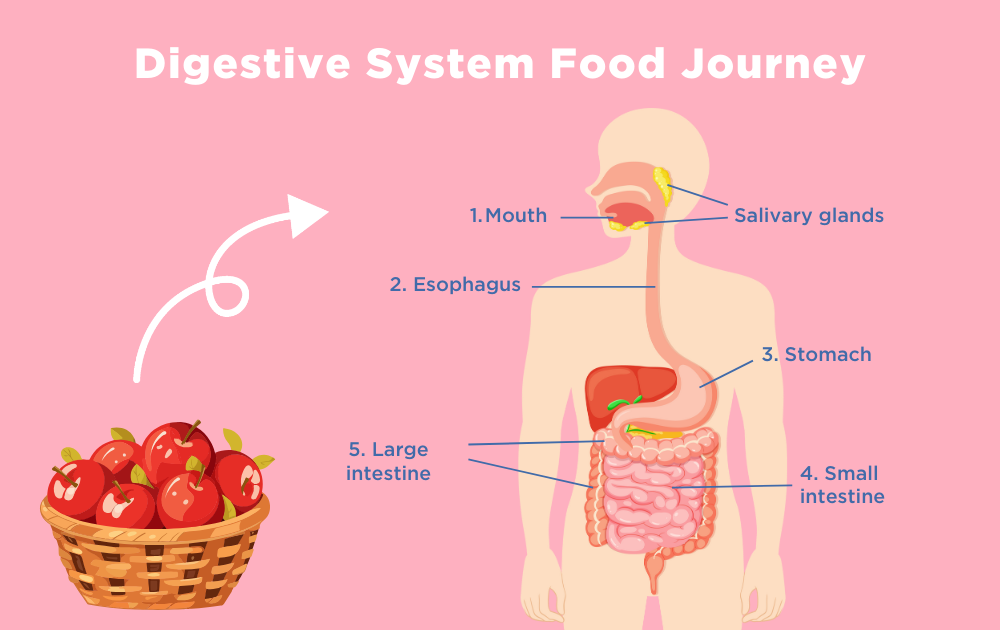
Chances are you’ve clicked on this blog to find out how we know if probiotics reach the right place in the body alive. To answer this question, we need to go back to a bit of basic biology. Imagine you’ve just taken a bite out of an apple…
Digestive enzymes in your saliva start to break down the starches and your teeth chew it into smaller pieces. These pieces travel down the esophagus into the stomach where its acidity breaks down the apple and kills some bacteria, helping to keep us healthy. Next, the apple pieces quickly travel through the small intestine where water and nutrients are absorbed. The large intestine has much slower transit times allowing the remaining water, salts, and nutrients to be absorbed before the stool moves on to end its journey in the body. The slower movement in the large intestine allows bacteria to colonize the intestinal walls. This is where undigested food particles can be broken down by bacteria allowing nutrients to be more easily absorbed by the body.
Now back to probiotics, depending on the microbial strains present in the food or capsule consumed, they will react differently to the harsh acidic conditions of the stomach. Most commercially sold probiotics have been chosen to withstand stomach acid. They don’t colonize in the small intestine because foods and fluids travel through much too quickly, and microbes don’t get a chance to make themselves comfortable. Although, this is a good thing! Sometimes, people can get infections in the small intestine such as by H. Pylori bacteria, or small intestinal bacterial overgrowth (SIBO) which is linked to slow gut motility – slow movement through the gut (11). Interestingly, studies indicate that up to 80% of people with IBS could have SIBO which is a treatable condition (12).
The Ultimate Proof – Do Probiotics Work For You?
A quick recap on what we know so far: probiotics are usually aimed at large intestine, eating whole foods with dietary fiber helps beneficial bacteria multiply and those microbes release key healthy compounds when they breakdown fiber. But how do we really know they got to the right place? The most valuable resource here is you! Pay attention to how you feel over time, not just on a one-off. Can you notice patterns in gut symptoms?
Gut health is unique to every individual and can change over time, so paying attention to your symptoms can help you discover if probiotics are working for you. Before trying anything new, make sure to speak to your doctor, especially if you are taking any other medications or supplements. Tests you can do to see into the gut include stool tests and breath tests. A stool sample can provide a snapshot in time based on the microbes that make it there whereas breath tests rely on the gases that bacteria and other microbes produce when they break down our food. Breath tests are often used to diagnose intolerances or conditions like SIBO. Yet one-off tests cannot track changes over time.

OMED Health has developed a wireless hydrogen and methane breath analyzer that connects to our mobile app via Bluetooth. This user-friendly technology allows you to take breath samples at key moments, such as before and after meals or when symptoms occur. With regular use, you can monitor changes in your gut microbiome and begin to understand how it responds to different foods and activities.
Through OMED Health Gut Reset+, we provide a clinically guided pathway that supports you before, during, and after a formal diagnosis from a doctor. Your breath test results can help inform a medical diagnosis of conditions such as SIBO (Small Intestinal Bacterial Overgrowth) or IMO (Intestinal Methanogen Overgrowth). Based on that diagnosis, we help guide you through appropriate treatment options and offer continued support to manage symptoms and improve your gut health over time.
References
- Hamasalim HJ. The Impact of Some Widely Probiotic (Iraqi Probiotic) on Health and Performance. Journal of Biosciences and Medicines. 2015 Aug 5;3(8):25–36. doi: 10.4236/jbm.2015.38003
- Xiong RG, Zhou DD, Wu SX, Huang SY, Saimaiti A, Yang ZJ, et al. Health Benefits and Side Effects of Short-Chain Fatty Acids. Foods. 2022 Sep 15;11(18):2863. doi: 10.3390/foods11182863
- Vieira AT, Galvão I, Macia LM, Sernaglia ÉM, Vinolo MAR, Garcia CC, et al. Dietary fiber and the short-chain fatty acid acetate promote resolution of neutrophilic inflammation in a model of gout in mice. J Leukoc Biol. 2017 Jan;101(1):275–84. doi: 10.1189/jlb.3A1015-453RRR
- Yang W, Yu T, Huang X, Bilotta AJ, Xu L, Lu Y, et al. Intestinal microbiota-derived short-chain fatty acids regulation of immune cell IL-22 production and gut immunity. Nat Commun. 2020 Sep 8;11(1):4457. doi: 10.1038/s41467-020-18262-6
- Han R, Nusbaum O, Chen X, Zhu Y. Valeric Acid Suppresses Liver Cancer Development by Acting as a Novel HDAC Inhibitor. Mol Ther Oncolytics. 2020 Dec 16;19:8–18. doi: 10.1016/j.omto.2020.08.017
- Zou J, Reddivari L, Shi Z, Li S, Wang Y, Bretin A, et al. Inulin Fermentable Fiber Ameliorates Type I Diabetes via IL22 and Short-Chain Fatty Acids in Experimental Models. Cell Mol Gastroenterol Hepatol. 2021;12(3):983–1000. doi: 10.1016/j.jcmgh.2021.04.014
- Chen Y, Xu C, Huang R, Song J, Li D, Xia M. Butyrate from pectin fermentation inhibits intestinal cholesterol absorption and attenuates atherosclerosis in apolipoprotein E-deficient mice. J Nutr Biochem. 2018 Jun;56:175–82. doi: 10.1016/j.jnutbio.2018.02.011
- Satokari R. High Intake of Sugar and the Balance between Pro- and Anti-Inflammatory Gut Bacteria. Nutrients. 2020 May;12(5):1348. doi: 10.3390/nu12051348
- Bustos Fernández LM, Man F, Lasa JS. Impact of Saccharomyces boulardii CNCM I-745 on Bacterial Overgrowth and Composition of Intestinal Microbiota in Diarrhea-Predominant Irritable Bowel Syndrome Patients: Results of a Randomized Pilot Study. Digestive Diseases. 2023 Jan 11;41(5):798–809. doi: 10.1159/000528954
- García-Collinot, G., Madrigal-Santillán, E.O., Martínez-Bencomo, M.A. et al. Effectiveness of Saccharomyces boulardii and Metronidazole for Small Intestinal Bacterial Overgrowth in Systemic Sclerosis. Dig Dis Sci 65, 1134–1143 (2020). doi: 10.1007/s10620-019-05830-0
- Sachdev AH, Pimentel M. Gastrointestinal bacterial overgrowth: pathogenesis and clinical significance. Therapeutic Advances in Chronic Disease. 2013 Sep 1;4(5):223–31. doi: 10.1177/2040622313496126
- Cleveland Clinic [Internet]. [cited 2024 May 28]. SIBO (Small Intestinal Bacterial Overgrowth): Symptoms, Diet, Causes & What it Is. Available from: https://my.clevelandclinic.org/health/diseases/21820-small-intestinal-bacterial-overgrowth-sibo