The gut microbiome is a community of microbial organisms that live in our gastrointestinal tract and coexist with us in a mutually beneficial relationship. These microorganisms play a pivotal role in our overall health, especially in shaping our immune system. This means that good gut health can help boost your immunity.
But how can we investigate this intricate relationship? Many molecules produced by the gut microbiome can be measured in exhaled breath and can inform us about the interactions between our microbiome and immune system.
The Impacts of our Microbiome on our Immune System, Health and Disease
Our gut is constantly exposed to the environment including through what we eat and drink. The “good” microbes in our gut microbiome are in frequent competition with potentially “bad” microorganisms as they both compete for space and nutrients in our gut. As such, our microbiomes have evolved to fend off pathogens and disease-causing microbes and “educate” the immune system so that we maintain a healthy balanced gut. This has created a mutual relationship between our immune system and microbiome, controlled by a variety of complex chemical signals and interactions. This relationship is complicated by the effect of our diet which may alter these interactions1.
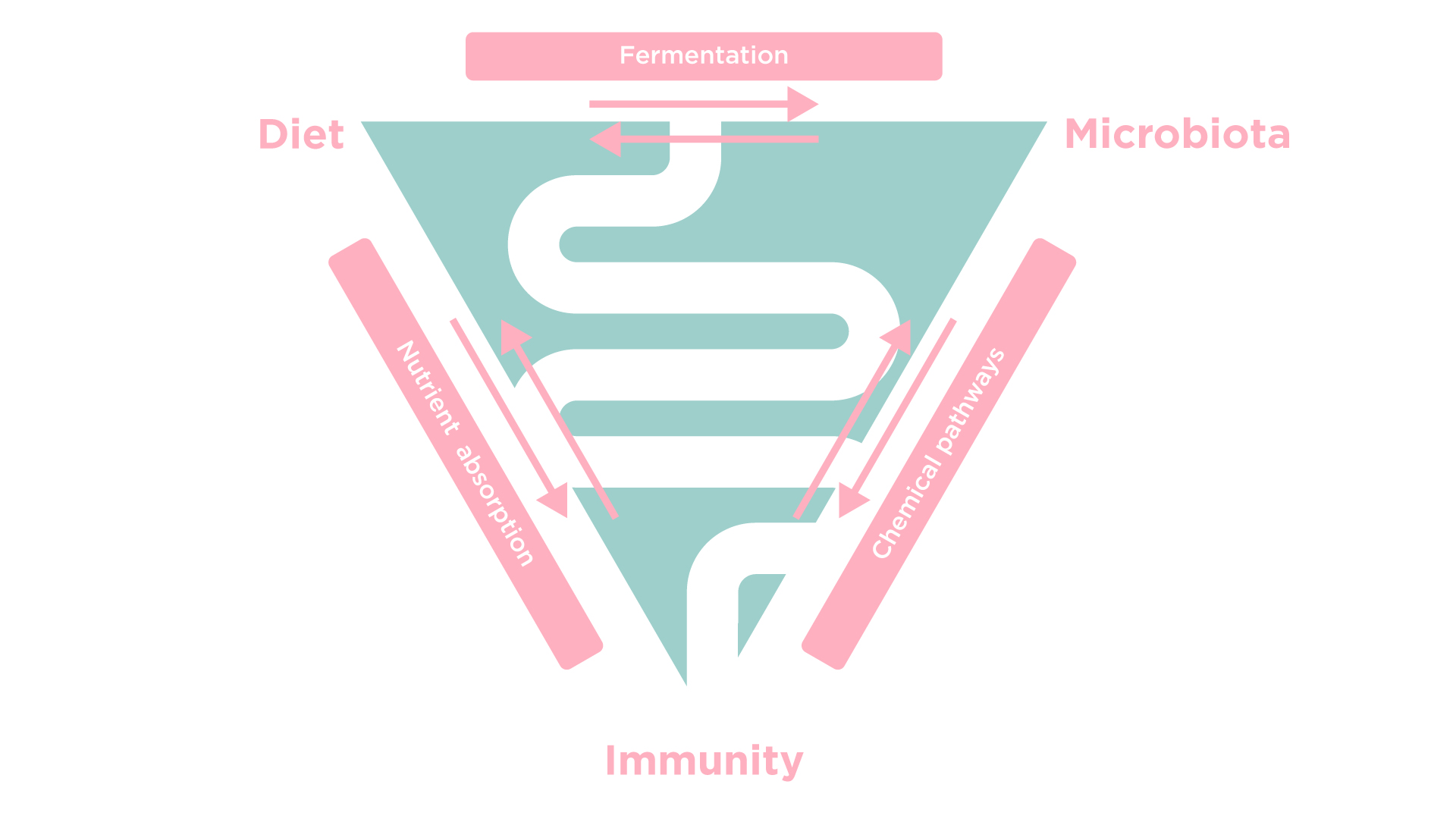
Some key molecules that regulate our immunity are short-chain fatty acids (SCFAs). These are produced through the fermentation of fiber by our “good” bacteria, in the intestines. Many of these SCFAs can be measured in breath and they can improve the activity of our immune cells, improve the protection of the gut barrier, and reduce inflammation. In fact, SCFAs can also contribute to the suppression of autoimmune diseases2.
Dysbiosis (where our microbiome is out of balance) can reduce SCFA production, which in turn adversely affects immune function. An altered microbiome may also produce harmful and inflammatory molecules that can increase the permeability of the intestinal barrier. These molecules have been linked to inflammatory bowel disease (IBD) and autoimmune diseases1, 2.
Gut dysbiosis has been recorded in type 1 diabetes patients. SCFAs usually shield the pancreas from damage caused by inflammatory molecules. However, people deficient in SCFAs are at a higher risk of an autoimmune response. Notably, abnormal SCFA levels and irregular microbiome diversity have been reported in various autoimmune diseases including rheumatoid arthritis, lupus, and multiple sclerosis, amongst others, reflecting the microbiome’s influence extending beyond solely gut health2.

Implications for Treatment and Research
A greater understanding of the interactions between the microbiome and the immune system could help with developing diagnostics and treatment options. As described in the examples above, SCFAs have significant effects on health and disease. Therefore, medications that target SCFA-producing microbes could be a potential treatment for these conditions.
However, the complexity of interactions affected by SCFAs and differences between individuals could lead to treatments being unsuccessful or harmful. Everyone’s microbiome is unique so a treatment that helps one person may not work for another. Therefore, further research on understanding the link between the microbiome, diet, and the immune system is required2.
Breath analysis provides a non-invasive technique for molecules like SCFAs to be measured. It can provide highly sensitive real-time analysis in response to various factors such as diet3 or medication and is well tolerated by patients, therefore suited for longitudinal monitoring and the early detection of disease.
At OMED Health, we are researching the microbiome, how it reacts to various nutritional stimuli, and identifying molecules associated with disease in order to develop clinical tests. Our upcoming OMED Health Breath Analyzer and App is one such device. This is a portable breath tester that allows you to record hydrogen and methane gas present in your breath. By evaluating these gases in conjunction with your symptoms, our experts can decipher potential causes and come up with a personalized plan to help. If you are interested in receiving updates about our newest device, you can sign up for the waitlist below.
References:
- Belkaid Y, Hand TW. Role of the microbiota in immunity and inflammation. Cell. 2014 Mar 27;157(1):121-41. doi: 1016/j.cell.2014.03.011.
- Kim CH. Complex regulatory effects of gut microbial short-chain fatty acids on immune tolerance and autoimmunity. Cell Mol Immunol. 2023 Apr;20(4):341-350. doi: 1038/s41423-023-00987-1.
- Neyrinck AM, Rodriguez J, Zhang Z, Nazare JA, Bindels LB, Cani PD, Maquet V, Laville M, Bischoff SC, Walter J, Delzenne NM. Breath volatile metabolome reveals the impact of dietary fibres on the gut microbiota: Proof of concept in healthy volunteers. EBioMedicine. 2022 Jun;80:104051. doi: 1016/j.ebiom.2022.104051