You may have heard that reducing dairy, or sugary foods can help get rid of acne, but is the gut-skin connection real? As is often the case with specific claims, there is mixed evidence. Yet, research shows there may be some truth them. Let’s dive into the science and figure out why diet and gut health could impact your skin.
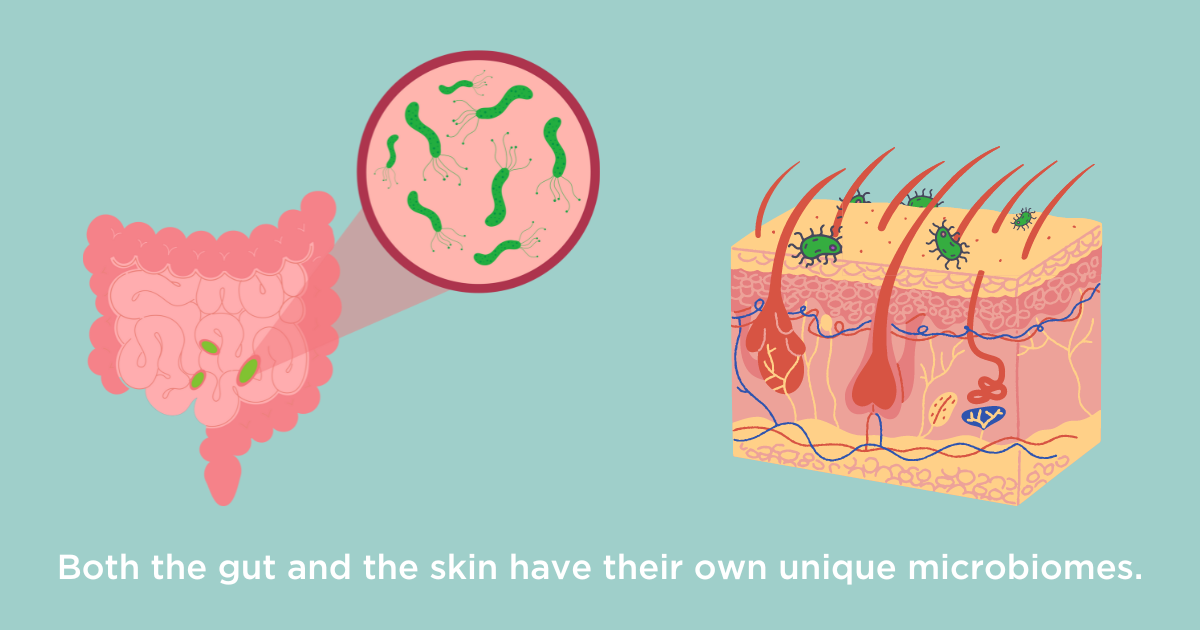
One key player behind the connection between the gut and the skin is the microbiome. This is the plethora of tiny organisms that live on your skin and in your body. The largest and most diverse colonies of bacteria and other microbes inhabit your gut. You may be wondering why the gut microbiome is so important. Part of the answer lies in the anatomy and function of the gut, which is surprisingly similar to that of the skin.
The gut and the skin are organs that play key roles due to their exposure to the outside world. The skin acts as a protective barrier, keeping dirt, pathogens, and more out, as well as keeping water in. The barrier function of the skin is shared by the gut. For example, the cells that are on the outer layer of the skin and the inner layer of the gut produce antimicrobial chemicals, preventing pathogens from entering the body. For both the gut and the skin, certain compounds are able to cross the barrier (1). In the gut, this element of permeability allows us to absorb nutrients from our food. In the large intestine, microbes that feed on dietary fiber can produce beneficial compounds that have been found to reduce inflammation and help regulate the immune system (2). On the skin, the permeability allows for the active ingredients in ointments or creams to be applied topically and absorbed into the deeper layers of the skin.
Both organs are also connected to many nerves, immune cells, and blood vessels which play a pivotal role in their function. Nerves allow us to feel something as delicate as the touch of a feather on the skin but can also make cause some people to feel painful cramps in response to stress and anxiety. Just as you might flush a bright red hue in an embarrassing moment, you may also feel your stomach churn. Yet these connections are not short-lived. Remarkably, recent research is finding significant links between gut problems and skin conditions such as psoriasis
Psoriasis is a skin rash that usually presents with red lesions and scaly dry skin (4). It develops due to a multitude of reasons including genetic predisposition, lifestyle choices and environmental factors. Although only around 2% of people living in the United States have psoriasis (5), studies have shown that up to 11% of people with inflammatory bowel disease (IBD) also have psoriasis (6). In case you were thinking this connection only went in one direction, people with psoriasis are more likely to develop gut disorders like IBD or celiac disease (7). The reasons behind this aren’t that clear, but we do know that inflammatory disorders like psoriasis and IBD are linked to the microbiome.

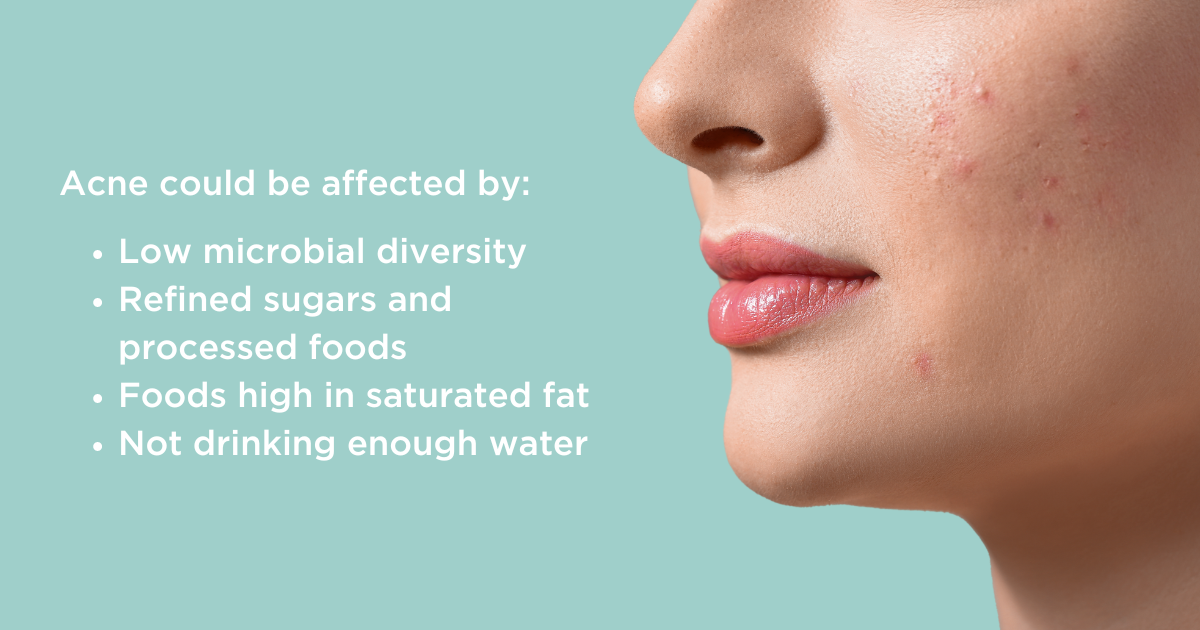
The skin microbiota of people with facial and back acne has been found to have less diversity of certain skin bacteria species and an increased number of particular group within that type of bacteria (8). On top of that, studies have found that people with acne may have altered gut microbiomes. Acne has also been linked to diets high in saturated fat which is why too much dairy could be an issue for you. Refined sugars have also been found to promote the growth of bacteria related to acne (9). This suggests that treating gut symptoms may help clear your skin.
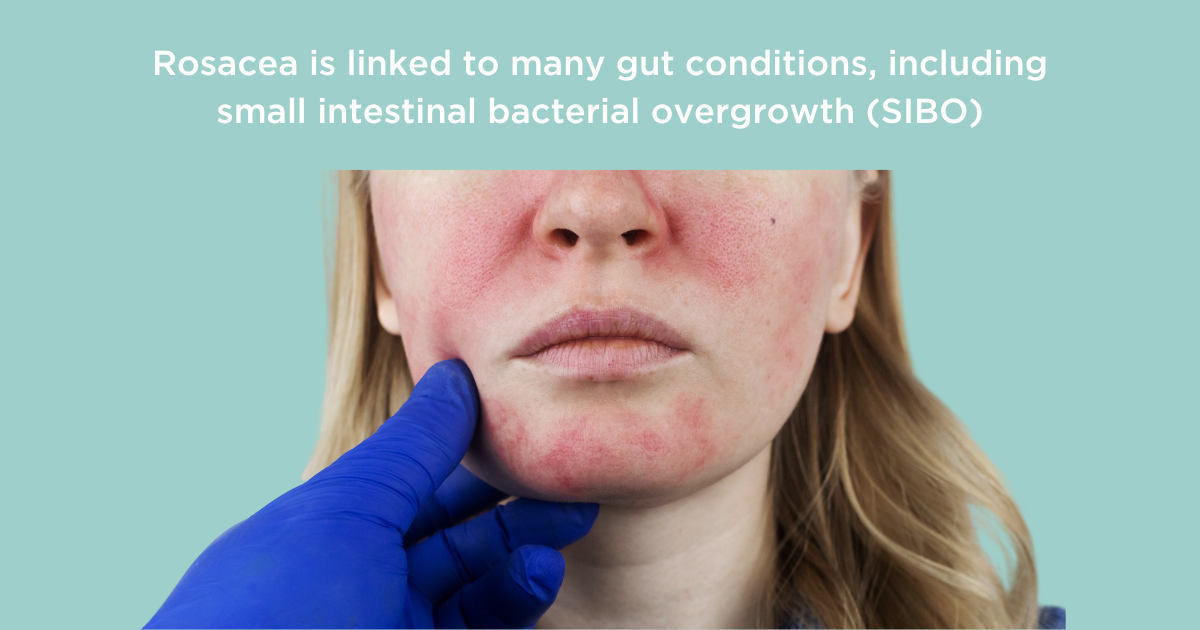
Rosacea is another skin condition that is characterized by facial redness, skin roughness, and pustules. It has now been linked to all kinds of inflammatory gut disorders including Crohn’s disease, celiac disease, ulcerative colitis, and inflammatory bowel syndrome(10) . Rosacea has also been shown to be more common in people with small intestinal bacterial overgrowth (SIBO) (11). This happens when microbes that shouldn’t really be in your small intestine make it their home. In one study on rosacea patients, it was found that over half of them also have SIBO (compared to only 3 out of 60 non-rosacea patients), and 26 of 28 patients who were successfully treated for SIBO with the antibiotic rifaximin also had marked improvements in their rosacea symptoms. You can read more about this study and SIBO-rosacea connection here. It’s important to remember that treatment of this condition could help your skin, but of course there is no guarantee as everyone’s body is unique and may react differently.
Our new at-home breath analyzer can help you monitor your gut microbiome alongside your gut health symptoms to identify whether lifestyle factors such as stress, or diet, are having an impact. The app allows you to keep track of those symptoms whilst also being able to see real-time methane and hydrogen levels from your breath. These are produced by your gut microbiome and high levels tend to coincide with how you feel. When carefully reviewed by our gut experts, the app can help you manage your gut condition and feel in control again. Using this tool, you can also monitor whether there is a connection between your skin and your gut health in tandem.
In conclusion, it’s difficult to say whether your gut issues are causing your skin problems, (or perhaps even the other way around), yet the research shows that the gut and the skin do interact in many ways. This means that if something isn’t working as well as it should be, this could have knock-on effects across the body, including the skin.
References:
- Shaykhiev R, Bals R. Interactions between epithelial cells and leukocytes in immunity and tissue homeostasis. J Leukoc Biol. 2007 Jul;82(1):1–15. doi:10.1189/jlb.0207096
- Xiong RG, Zhou DD, Wu SX, Huang SY, Saimaiti A, Yang ZJ, et al. Health Benefits and Side Effects of Short-Chain Fatty Acids. Foods. 2022 Sep 15;11(18):2863. doi: 10.3390/foods11182863
- Vlachos C, Gaitanis G, Katsanos KH, Christodoulou DK, Tsianos E, Bassukas ID. Psoriasis and inflammatory bowel disease: links and risks. PTT. 2016 Jul 20;6:73–92. doi: 10.2147/PTT.S85194
- nhs.uk [Internet]. 2017 [cited 2024 May 14]. Psoriasis. Available from: https://www.nhs.uk/conditions/psoriasis/
- Psoriasis: Causes [Internet]. [cited 2024 May 14]. Available from: https://www.aad.org/public/diseases/psoriasis/what/causes
- Huang BL, Chandra S, Shih DQ. Skin Manifestations of Inflammatory Bowel Disease. Front Physiol [Internet]. 2012 Feb 6 [cited 2024 May 14];3. Available from: https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2012.00013/full. https://doi.org/10.3389/fphys.2012.00013
- Pietrzak D, Pietrzak A, Krasowska D, Borzęcki A, Franciszkiewicz-Pietrzak K, Polkowska-Pruszyńska B, et al. Digestive system in psoriasis: an update. Arch Dermatol Res. 2017 Nov;309(9):679–93. doi: 10.1007/s00403-017-1775-7
- Dréno B, Dagnelie MA, Khammari A, Corvec S. The Skin Microbiome: A New Actor in Inflammatory Acne. Am J Clin Dermatol. 2020 Sep 1;21(1):18–24. https://doi.org/10.1007/s40257-020-00531-1
- Mahmud MdR, Akter S, Tamanna SK, Mazumder L, Esti IZ, Banerjee S, et al. Impact of gut microbiome on skin health: gut-skin axis observed through the lenses of therapeutics and skin diseases. Gut Microbes. 2022 Dec 31;14(1):2096995.
- Mann EA, Bae E, Kostyuchek D, Chung HJ, McGee JS. The Gut Microbiome: Human Health and Inflammatory Skin Diseases. Ann Dermatol. 2020 Aug;32(4):265–72.
- Sánchez-Pellicer P, Eguren-Michelena C, García-Gavín J, Llamas-Velasco M, Navarro-Moratalla L, Núñez-Delegido E, et al. Rosacea, microbiome and probiotics: the gut-skin axis. Front Microbiol. 2024 Jan 8;14:1323644. doi: 10.3389/fmicb.2023.1323644






