Have you ever had a gut feeling about something? Felt butterflies in your stomach in an exciting situation? Experienced nausea when anxious about an upcoming event? These are all examples of the connections between our gut and our brain through the gut brain axis, a complex network of neural and chemical pathways that allow for communication between our gut and our brain. These communication pathways allow many different emotions or feelings to affect the gut and equally allow many of the changes to the gut and its environment to affect our mental state.
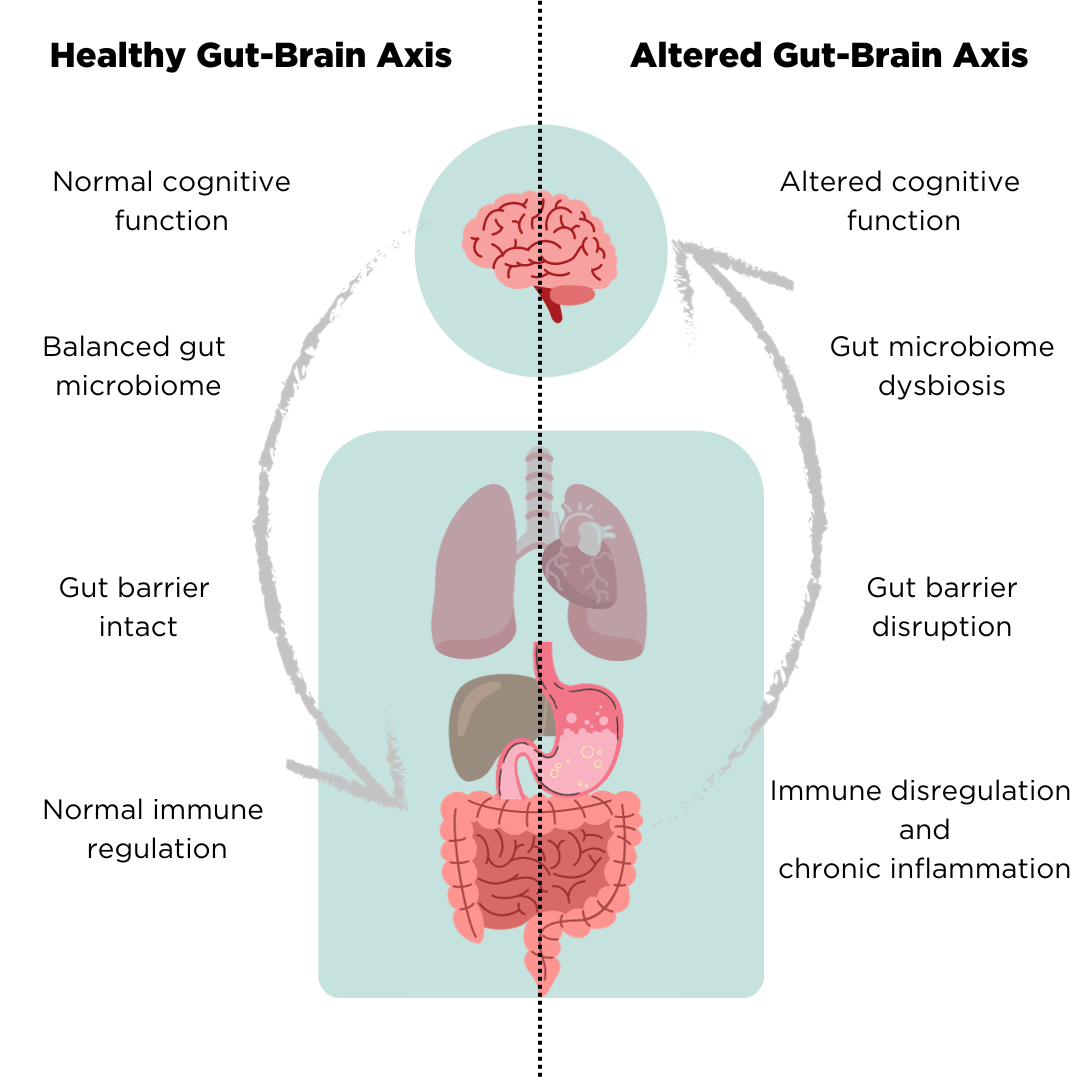
The effects that the gut-brain axis can have on our body are profound. In a healthy system where the axis is working in harmony, the immune system is well regulated, cognitive factors remain normal and the microbiome of the gut remains balanced. Disruption of the gut-brain axis can result in harmful effects on the body and may be implicated in a range of different diseases.
In functional gut diseases, such as IBS, the link between the gut and the brain has long been established. Almost 85% of patients report anxiety or depression as conditions alongside their IBS diagnosis, so much so that it was previously almost believed to be an entirely psychosomatic condition (1). Importantly, the gut and brain connection is bi-directional, meaning that just as alterations to the gut can influence the brain, alterations in the brain can influence the gut. This means that mental disorders or feelings of anxiety may be either a trigger or a product of various gastrointestinal diseases.
Psychological stress is one mental factor that has been shown to exacerbate gut inflammation in specific bowel diseases. This process is driven by stress hormones, known as glucocorticoids, being released from the brain. A recent publication by Schneider et al. has shed light on this process, showing that when certain cells supporting the nervous system in the gut (glial cells) are targeted by these stress hormones, they release molecules that activate the immune system, which subsequently trigger inflammation in the local area (2). Increases in inflammation can cause the development or worsening of symptoms of a range of different bowel diseases, including IBS.
Gut Brain Axis – Microbiome.
The microbiota, the community of microorganisms unique to every human, is one of the key components of the gut brain axis – its influence is so significant that it is often combined to form the term microbiota-gut-brain axis. Disruption to the gut microbiota can affect behavior and mood through this axis, and the bidirectional communication means that changes in the brain, such as behavior and mood, can also affect the microbiota and the gut.
Having a disrupted or imbalanced microbiota can have a range of effects, including the activation of the immune system and the disruption of the gut barrier. These can contribute to many inflammatory gut diseases, such as IBS. Disruption of the microbiota can also cause inflammation in the gut, leading to the release of inflammatory and neuroactive substances which can then travel to the brain through the various communication pathways, causing changes in behavior and mood.
The Two-Way Street Between the Gut Brain Axis and Mental Health.
As previously mentioned, mental disorders may also be the product of disruption to the gut, for example by a dysregulated microbiome. This means that treating your gastrointestinal issues can simultaneously improve your mental health, just as treating mental disorders can improve the symptoms of gastrointestinal diseases. As an example, symptoms associated with major depressive disorder have been shown to improve through treatment with probiotics which aim to manipulate the microbiome of the gut (3).
As with mental health disorders and different treatments such as probiotics, identifying the link between the gut and the brain has led to alternative treatments being tested for gastrointestinal diseases, with many positive outcomes. For example, research has shown that treatment by cognitive behavioural therapy (CBT) can greatly reduce the severity of symptoms in IBS sufferers after 12 months of treatment in comparison to those receiving standard IBS treatments (4). Further research has shown that patients suffering from functional gut disorders may see improvements in the condition through the treatment of anxiety, given that anxiety is one of many possible triggers of functional gut diseases (5).
To determine whether anxiety or other mental conditions may be impacting your gut health, it is important to continuously monitor mental symptoms alongside physical symptoms to unveil potential links. For example, by tracking your emotions and mental state, you may discover that feelings of anxiousness or sadness occur most frequently or at a greater severity alongside worsening of gastrointestinal symptoms. Revealing connections between these symptoms can then be used to optimize the treatments that you are receiving, targeting possible mental triggers to improve the chance of success in treating your gastrointestinal health.
OMED Health – Your Tool For Exploring the Gut-Brain Axis.
The OMED health app allows you to track mental symptoms alongside physical symptoms of gastrointestinal disease to determine whether there are connections between them and provides insights into the possible influences of the microbiome via recording hydrogen and methane levels. Hydrogen and methane levels are important indicators for the state of your gut microbiome and can be determined using our soon–to–be–released OMED health breath analyzer. The analyzer relays your hydrogen and methane measurements directly to the OMED health app, meaning that all data relating to the state of the microbiome, mental symptoms, and physical symptoms can be stored in one convenient place.
By analyzing the data collected, connections can be determined between your physical symptoms, mental symptoms, and the state of your gut microbiome, informing you of potential triggers for your gastrointestinal disease. Using our platform of connected physicians, you can use this information to make well-informed decisions about the best treatment options available for you to ensure the highest chance of successfully treating your symptoms. The success of treatments can also be determined through the continued monitoring of your symptoms and microbiome state on the OMED health app, allowing you to visualize gut health improvement over a period of time, or switch to an alternative treatment method if necessary.
Hydrogen methane breath test kits (HMBTs) are also available for those who think they may be suffering from small intestinal bacterial overgrowth or food intolerances, conditions that may also be influenced by the gut-brain axis. These easy-to-use test kits can be completed from your home and can be used to help pinpoint the underlying cause of uncomfortable digestive symptoms. You can find out how to refer yourself for our at-home breath testing kits here.
References
- Kawoos Y, Wani ZA, Kadla SA, Shah IA, Hussain A, Dar MM, et al. Psychiatric Co-morbidity in Patients With Irritable Bowel Syndrome at a Tertiary Care Center in Northern India. J Neurogastroenterol Motil. 2017 Oct 31;23(4):555–60. DOI: 10.5056/jnm16166
- Schneider KM, Blank N, Alvarez Y, Thum K, Lundgren P, Litichevskiy L, et al. The enteric nervous system relays psychological stress to intestinal inflammation. Cell. 2023 Jun 22;186(13):2823-2838.e20. DOI: https://doi.org/10.1016/j.cell.2023.05.001
- Wallace CJK, Milev R. The effects of probiotics on depressive symptoms in humans: a systematic review. Ann Gen Psychiatry. 2017 Feb 20;16:14. DOI: 10.1186/s12991-017-0138-2
- Everitt HA, Landau S, O’Reilly G, Sibelli A, Hughes S, Windgassen S, et al. Assessing telephone-delivered cognitive–behavioural therapy (CBT) and web-delivered CBT versus treatment as usual in irritable bowel syndrome (ACTIB): a multicentre randomised trial. Gut. 2019 Sep 1;68(9):1613–23. DOI: 10.1136/gutjnl-2018-317805
- Thiwan SIM, Drossman DA. Treatment of Functional GI Disorders With Psychotropic Medicines: A Review of Evidence With a Practical Approach. Gastroenterol Hepatol. 2006 Sep;2(9):678–88. DOI: PMC5350580

